
Springfield community
The Springfield Community includes Christian, Greene and Webster counties in Missouri.

PART 1: Introduction

PART 1: Introduction
Executive Summary
Since 2016, hospital systems, local public health agencies (LPHAs) and other health care partners in the greater Ozarks have worked together to release comprehensive Community Health Needs Assessments (CHNAs) every three years. This group, known as the Ozarks Health Commission (OHC), released community-level reports in 2016, 2019 and 2022. For the fourth iteration, the 2025 assessment has been compiled into community-level and regional snapshots, continuing the regional scope introduced in 2022.
Health care partners and LPHAs develop the results of these assessments into Community Health Improvement Plans (CHIPs). Organizations use CHIPs to target areas of health need and disparity in communities and create actionable plans to make them better over time.
The scope of the OHC region includes 33 counties across three states. These counties make up seven different communities, who each develop reports based on their community-level data. Information about data collection can be found in the OHC Regional Report.
The following is the 2025 Springfield Community CHNA. This report aims to be a valuable resource for health care partners, civic organizations and people who live, work and seek health care in the Springfield Community.

Service Area
The Springfield Community includes Christian, Greene and Webster counties in Missouri. It encompasses the service areas of Mercy Hospital Springfield, CoxHealth, the Springfield-Greene County Health Department, the Christian County Health Department, the Webster County Health Unit and Burrell Behavioral Health.
More than 428,000 residents call the Springfield Community home. Between 2010 and 2020, the total population increased by 10%. The growth of the Springfield Community defies the population stagnation or decline in most other CHNA communities within the last decade. Springfield growth also outpaces Missouri, which grew just under 3% from 2010 to 2020.

Population overview
The Springfield Community population is evenly split between men and women. 74% of the population live in urban areas, while 26% live in rural areas.
Of the total population in the Springfield Community, 22% are under the age of 18, 61% are between the ages of 18-64, and 17% are age 65 or older.
The majority of Springfield Community residents (88%) identify as non-Hispanic White. Just over 2% identify as non-Hispanic Black. About 4% of residents identify as Hispanic or Latino. Almost 2% identify as non-Hispanic Asian and 4% identify as non-Hispanic multiple races.
Top 10 languages spoken in the Springfield community
LANGUAGE |
|---|
English |
Spanish |
German/West Germanic languages |
Indo-European languages |
Russian, Polish or other Slavic languages |
Asian and Pacific Islander languages |
Other/unspecified languages |
Mandarin and Cantonese |
Vietnamese |
Tagalog (incl. Filipino) |
Population by age
.png)
Population by race and ethnicity
.png)
Rural vs. urban population
.png)
Root causes
Each person’s health and health care paths are different, but there are certain root causes that can contribute to poor health outcomes. Things like access to medical care, financial stability and stigma toward certain conditions can prevent a person from taking preventative actions for their health, seeking care or changing their lifestyle.
The following root causes are most frequently cited in the Springfield Community as barriers to health:

Access to care
DEFINITION
Access to care is the ability and ease for a person to receive timely, appropriate, local health services. It impacts nearly all health issues.¹
IMPACT IN SPRINGFIELD COMMUNITY
Community members most often cite scheduling difficulties, lack of awareness about available resources and finances as their largest barriers to accessing health care.
The Springfield Community is a major health care hub in the region, especially in Greene County. This concentration of services is beneficial for access overall. However, it can lead to gaps in access for rural populations within their communities and an overwhelming demand within Greene County. This is especially true for mental health care.
Non-health care costs
DEFINITION
Living costs can influence a person’s ability to prioritize healthy choices.² Individuals may have to choose between paying for housing, childcare, or transportation over preventative health care expenses or nutritious foods.
IMPACT IN SPRINGFIELD COMMUNITY
Transportation access and housing costs greatly affect the Springfield Community. Half of Springfield Community residents’ average household income is spent just on housing and transportation. For residents who rely on childcare outside of the home, these costs amount to 28% of household income on average. These cost burdens directly impact health in the Springfield Community.
Access to care
DEFINITION
Access to care is the ability and ease for a person to receive timely, appropriate, local health services. It impacts nearly all health issues.¹
IMPACT IN SPRINGFIELD COMMUNITY
Community members most often cite scheduling difficulties, lack of awareness about available resources and finances as their largest barriers to accessing health care.
The Springfield Community is a major health care hub in the region, especially in Greene County. This concentration of services is beneficial for access overall. However, it can lead to gaps in access for rural populations within their communities and an overwhelming demand within Greene County. This is especially true for mental health care.
Non-health care costs
DEFINITION
Living costs can influence a person’s ability to prioritize healthy choices.² Individuals may have to choose between paying for housing, childcare, or transportation over preventative health care expenses or nutritious foods.
IMPACT IN SPRINGFIELD COMMUNITY
Transportation access and housing costs greatly affect the Springfield Community. Half of Springfield Community residents’ average household income is spent just on housing and transportation. For residents who rely on childcare outside of the home, these costs amount to 28% of household income on average. These cost burdens directly impact health in the Springfield Community.
Physical activity
DEFINITION
Exercise is vital for overall health. Lack of physical activity or access to exercise opportunities can lead to negative health outcomes, including poor mental and heart health.³
IMPACT IN SPRINGFIELD COMMUNITY
One in ten residents report that they have not been physically active within the last 12 months. The rate of fitness and recreation facilities in the community are just below the overall rate for the state of Missouri. However, access in rural areas, especially to nearby parks, is lower when compared to urban areas of the Springfield Community.
Residents also noted chronic and mental health conditions as barriers to regular exercise and physical activity. These conditions can include symptoms like pain, low energy and difficulty breathing.
Nutrition
DEFINITION
A healthy and balanced diet is another factor that affects overall health. In adults, eating healthy foods can help maintain a healthy weight and lower the risk of heart disease, type 2 diabetes and some cancers.⁴
IMPACT IN SPRINGFIELD COMMUNITY
Transportation access and housing costs greatly affect the Springfield Community. Half of Springfield Community residents’ average household income is spent just on housing and transportation. For residents who rely on childcare outside of the home, these costs amount to 28% of household income on average. These cost burdens directly impact health in the Springfield Community.
Stigma
DEFINITION
Stigma refers to negative attitudes, beliefs, and stereotypes people may hold toward those who experience health conditions.⁵ Stigma can affect a person’s desire or ability to seek care.
IMPACT IN SPRINGFIELD COMMUNITY
Community members and partners frequently identify stigma as a barrier to seeking care and improving overall health. This is especially true in reference to mental health care and among historically marginalized populations.
Q: In the past 12 months, did you regularly eat healthy meals? If not, why?
“[We don’t always have] running water or propane.”
- Community Survey, 2024
Q: How does stigma impact a person’s health?
“[We must make sure] we’re creating welcoming spaces for people where they will actually seek out health care.”
- Community Leader, 2024

PART 2: Areas of focus
For the 2025 iteration of the CHNA, the Springfield Community chose to focus in-depth on two areas of focus: mental health and heart health. These two health issues rose to the top of the priority list due to prevalence and affected populations.
Each area of focus will dive into specific conditions and the populations in the Springfield Community who are most affected. Each condition will also contain attributions to their most common root causes, as defined in the previous section.
Mental health

Heart health
Other areas of interest
MENTAL HEALTH
ROOT CAUSES:
Access to care, stigma and non-health care costs.
Over the last decade, the Springfield Community has continually identified mental health and substance use as priority concerns. While the mental health provider to patient ratio is higher in the Springfield Community compared to the OHC region, the substance use provider to patient ratio is lower. In both instances, the demand for services outweighs available care.
Efforts to develop upstream care and support practices, along with stigma reduction efforts, have made a positive impact on mental health and substance use in the Springfield Community. However, people in nearly every demographic group experience poor outcomes at a greater rate than neighbors across the state and the OHC region.
Depression and anxiety
Suicide mortality
Substance use
Anxiety and depression
The Springfield Community shows higher rates of anxiety and depression than Missouri and the OHC region. Utilization of services for these conditions is 1.5 times higher in the Springfield Community than throughout the OHC region.
Anxiety and depression impact older adults at higher rates.
Rates of anxiety and depression by age

Anxiety and depression
The Springfield Community shows higher rates of anxiety and depression than Missouri and the OHC region. Utilization of services for these conditions is 1.5 times higher in the Springfield Community than throughout the OHC region.
Anxiety and depression impact older adults at higher rates.
Rates of anxiety and depression by age
.png)
Suicide mortality and ideation
The Springfield Community’s suicide mortality rate is unchanged since the 2022 CHNA and continues to be greater than the state and the OHC region. This is especially true for males.
In addition, diagnoses of suicidal ideation are high in the Springfield Community when compared to the OHC region and the state. Ideation includes having thoughts or plans of completing suicide. Rates of suicidal ideation are highest among Black individuals in the Springfield Community.
Generally, middle-aged adults in the Springfield Community are more likely to die by suicide, while younger adults are more likely to experience suicidal ideation. This indicates an opportunity for early interventions.
Male suicide mortality rate by age group
.png)
Substance use
Hospitalization due to drug use remains high in the Springfield Community compared to the OHC region and the state. In 2022, deaths from drug overdose in this community slightly decreased after a rapid increase in 2020.
In recent years, there has been an increased effort to combat high rates of drug overdose deaths. One result of these efforts is the widespread distribution of naloxone in the community. Naloxone is a medication that reverses the effects of opioid overdose.
Beyond opioids and other drugs, tobacco, marijuana, and alcohol use are also of notice in the Springfield Community.
Among middle and high school students surveyed in 2024, 8% reported recently using e-cigarettes. This is a slight decrease from 9% in 2022. During the same two-year period, youth alcohol consumption fell from 8% to 7%, but recent marijuana use increased from 4% to 6%.⁶
For adults, almost one in five in the Springfield Community are current smokers. Many adults also report excessive consumption of alcohol. The Springfield Community’s excessive drinking rate is slightly lower than Missouri’s. However, it is still concerning given the link between heavy alcohol use and poor health outcomes such as cancer, mental health conditions and heart disease.⁷
In 2023, there was 45 times more naloxone available in the Springfield Community than in 2018.
Heart HEALTH
ROOT CAUSES:
Access to care, nutrition and physical activity
Poor heart health is the leading cause of death for those living in the Springfield Community. While these conditions are often associated with the elderly population, the effects can be felt much earlier. Often, high blood pressure progresses to heart disease, and heart disease leads to heart failure.
Factors that can lead to poor heart health include age, race, family history, being overweight, and lifestyle factors like tobacco use or a lack of exercise. Addressing lifestyle factors early can improve outcomes and promote better overall health.

High blood pressure

ischemic heart disease

heart failure
High blood pressure
High blood pressure, or hypertension, is a common chronic condition that can be dangerous or life-threatening if untreated.
According to Mayo Clinic, the risk of developing high blood pressure increases with age. High blood pressure is more common in men until about age 64, and women are more likely to develop the condition beyond age 65. High blood pressure is also more common among Black people, for whom the condition tends to develop sooner in life.⁸
These population-based trends are reflected in the Springfield Community, where individuals who are over age 85, women or Black exhibited the highest rates of high blood pressure in hospital visits.


Ischemic heart disease
According to the American Heart Association, ischemic heart disease (also known as coronary artery disease or coronary heart disease) is heart damage caused by narrowed heart arteries. Narrowed arteries make it more difficult for blood and oxygen to reach the heart. This can cause chest pain or discomfort and lead to heart attack.⁹
Emergency department data shows that Springfield Community patients presented with ischemic heart disease at a rate exceeding the OHC region. Like many chronic conditions, ischemic heart disease acutely impacts older adults. Men also exhibit higher rates compared to women.
Heart health hospitalizations by gender
.png)
Heart health hospitalizations by age group
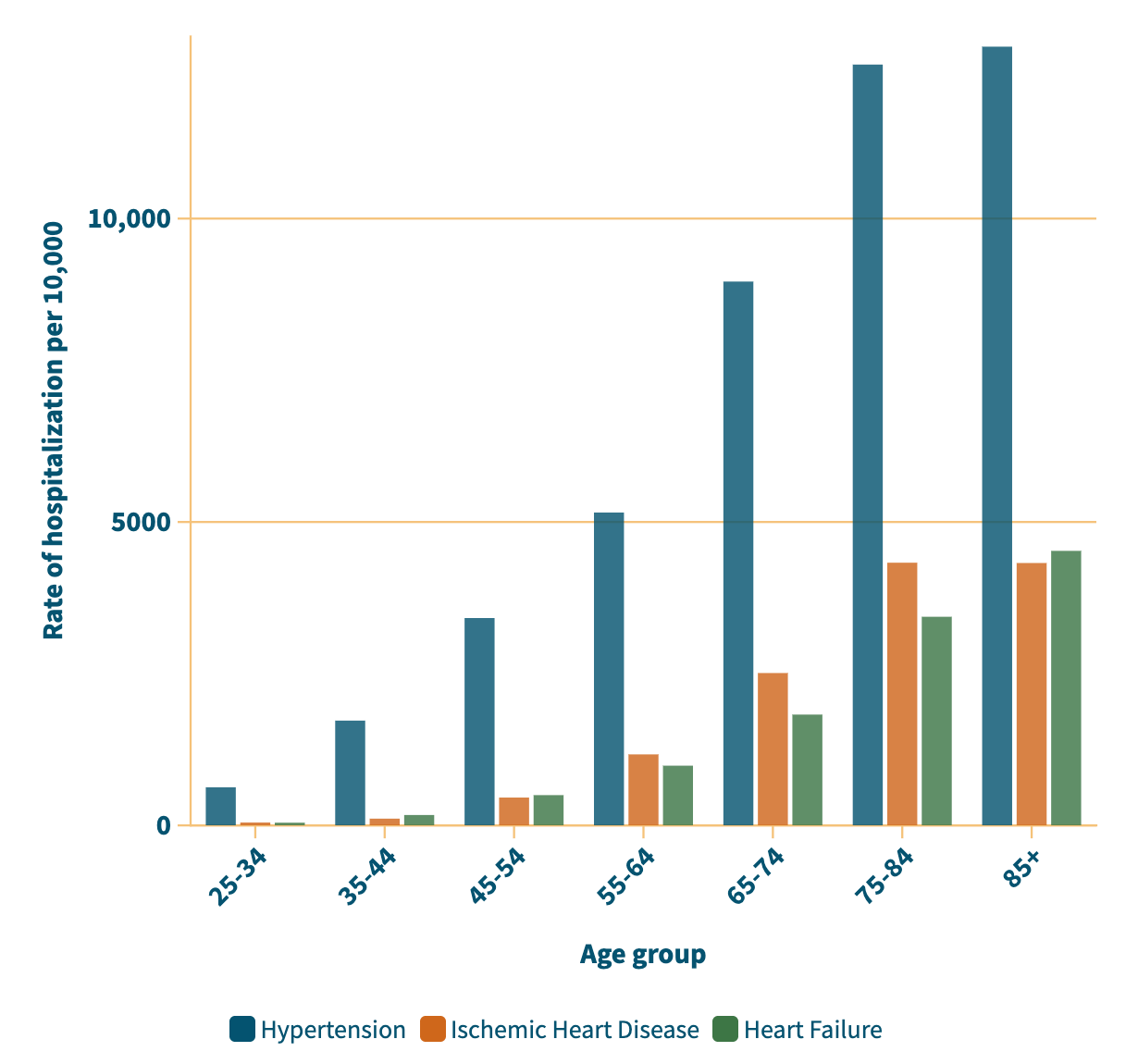
Heart failure
Heart failure is a condition that describes a weakened heart that is no longer able to keep up with its workload (American Heart Association). Individuals with heart failure experience symptoms such as fatigue, shortness of breath, and difficulty completing everyday activities like climbing stairs or carrying groceries. While there is usually no cure, many people with heart failure lead an enjoyable life when the condition is managed with medication and a healthy lifestyle.¹⁰


Community Feedback
Community partners were invited to a session to review the areas of focus. Partners were asked to identify populations within the Springfield Community most vulnerable to mental health and heart health conditions. Feedback primarily aligned with the data presented here. However, partners additionally called attention to those experiencing chronic stress, anxiety and social isolation, postpartum women, LGBTQ+ individuals, people experiencing poverty and unsheltered or unhoused individuals.
Other areas of interest
In addition to areas of focus for the Springfield Community, other conditions have been identified as areas of interest. These are public health issues for this community but are not an area of focus for this assessment. They are included to provide a broad snapshot of other conditions that affect the Springfield Community.

Cancer
respiratory illness

Sexually transmitted infections

Diabetes
Communicable disease
Vector-borne illness
Cancer
In the Springfield Community, cancer is the second leading cause of death.
Breast cancer rates are 124 per 100,000 females. This number is higher than the OHC region at 111 per 100,000 females.
Prostate cancer rates are 105 per 100,000 males. This number is higher than both the OHC region (92 per 100,000) and the state (96 per 100,000).

Diabetes
Diabetes was a priority health issue in the 2022 Springfield Community CHNA report.
There are three types of diabetes: Type 1, Type 2 and gestational.
Type 1 diabetes is most often genetic and diagnosed in childhood. In a three-year period, 82 per 10,000 people in the Springfield Community were treated for Type 1 diabetes. Type 2 has a genetic component but is more likely impacted by lifestyle factors.
In a three-year period, 1,466 per 10,000 people in the Springfield Community were treated for Type 2 diabetes.
Gestational diabetes can impact pregnant people. It is routinely screened for in the second trimester. In a three-year period, 22 per 10,000 people in the Springfield Community were treated for gestational diabetes.

Lung health
Chronic lung conditions including chronic obstructive pulmonary disease (COPD) and asthma are incurable and cause mild to severe breathing difficulties. The conditions may co-occur with other chronic ailments and contribute to poor health outcomes. COPD is often, but not always, associated with a history of smoking or tobacco exposure.
The Springfield Community exhibits higher rates for both asthma (670.3 per 10,000) and COPD (778.1 per 10,000) than the OHC region (463.9 per 10,000 – asthma, 754.9 per 10,000 – COPD), and higher rates of asthma than the state (566.5 per 10,000). In our community, asthma disproportionately impacts women, older adults and Black individuals. COPD rates are highest among older adults.

Communicable diseases
Communicable diseases spread from person to person, including respiratory illnesses. The severity of some of these illnesses can be reduced through vaccination.
Pertussis, also known as whooping cough, is a respiratory illness that is especially dangerous for infants, young children and people with pre-existing health conditions.
In 2023, there were fewer than 10 confirmed cases of pertussis. In 2024, more than 100 cases were confirmed (or probable) in the Springfield Community.

Sexually transmitted infections
Sexually transmitted infections (STIs) are spread through sexual contact. They are preventable and treatable.
Syphilis is a bacterial infection that develops in stages. Each stage of syphilis has different symptoms.
From 2019-2023, the rate of syphilis cases increased almost five times in the Springfield Community.
Human immunodeficiency virus (HIV) is a virus that attacks the body’s immune system. Without treatment, it can lead to acquired immunodeficiency syndrome (AIDS). HIV can also be spread through intravenous (IV) drug use.
In the Springfield Community, 170 per 100,000 people are living with HIV. HIV primarily affects Greene County.

Vector-borne illness
Engagement with the Springfield Community’s abundant outdoor resources comes with increased need for awareness and prevention of illnesses from insects, particularly Alpha-gal Syndrome (AGS), Lyme disease and ehrlichiosis.
AGS, Lyme disease and ehrlichiosis are caused by bites from infected ticks.
Tick-borne illnesses in Missouri are generally increasing.
While Alpha-gal is not a reportable condition, it is an important public health concern that is impacting Missourians.
%20(700%20x%20500%20px).png)

PART 3: Closing Remarks

Conclusion
While this overview of health in the Springfield Community is not comprehensive, it gives an important glimpse into areas of concern reflected in both data and community feedback. The 2025 assessment will be used to inform public health and health care initiatives. These initiatives will be outlined in a forthcoming Community Health Improvement Plan.
Dissemination
The OHC regional report and all community-level reports are available to the public through various channels
Websites
Printed copies
Printed copies will be available by request through health care partners and LPHAs. Please refer to organization websites or contact an organization directly
Health services available
Mercy Hospital Springfield
Seniorage Area Agency on Aging
Springfield-Greene County Health

acknowledgments
Thank you to Springfield Community partners and residents for contributing to this assessment through your feedback. Your contributions provide rich context to the vast health care data compiled for this report.
Thank you to the OHC Steering Committee for your collaboration and resource sharing during every step of the CHNA process.
Thank you to the Springfield Community representatives in the OHC Steering Committee for your contributions toward data collection and creation of the report.
Citations
¹ “Health Care Access and Quality.” U.S. Department of Health and Human Services, Office of
Disease Prevention and Health Promotion. https://odphp.health.gov/healthypeople/objectives-and-data/browse-objectives/health-care-access-and-quality.
² “Economic Stability.” U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://odphp.health.gov/healthypeople/objectives-and-data/browse-objectives/economic-stability.
³ “Benefits of Physical Activity.” Centers for Disease Control and Prevention. Last modified April 24, 2024. https://www.cdc.gov/physical-activity-basics/benefits/index.html.
⁴ “Benefits of Healthy Eating for Adults.” Centers for Disease Control and Prevention. Last modified February 14, 2024. https://www.cdc.gov/nutrition/php/resources/healthy-eating-benefits-for-adults.html.
⁵ “Mental Health Stigma.” Centers for Disease Control and Prevention. Last modified January 31, 2025. https://www.cdc.gov/mental-health/stigma/index.html.
⁶ “2024 Missouri Student Survey County Reports.” Missouri Department of Mental Health. https://dmhmo.gov/alcohol-drug/mobhew/missouri-student-survey-reports/2024.
⁷ “Facts About Excessive Drinking.” Centers for Disease Control and Prevention. Last modified October 7, 2024. https://www.cdc.gov/drink-less-be-your-best/facts-about-excessive-drinking/.
⁸ Mayo Clinic Staff. “High blood pressure (hypertension).” Mayo Clinic. Last modified February 29, 2024. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/
syc-20373410.
⁹ “Ischemic Heart Disease and Silent Ischemia.” American Heart Association. Last modified December 11, 2024. https://www.heart.org/en/health-topics/heart-attack/about-heart-attacks/silent-ischemia-and-ischemic-heart-disease.
¹⁰ “What is Heart Failure?.” American Heart Association. Last modified March 22, 2023. https://www.heart.org/en/health-topics/heart-failure/what-is-heart-failure.
